 A new study conducted by researchers at the University of Pittsburgh has found that dermatologists are most likely to discover melanomas in patients aged 50 years or older, and recommends the use of screenings for patients in this age group. A personal history of skin cancer or family history of melanoma also correlated with likelihood that melanoma will be discovered first by dermatologist screening.
A new study conducted by researchers at the University of Pittsburgh has found that dermatologists are most likely to discover melanomas in patients aged 50 years or older, and recommends the use of screenings for patients in this age group. A personal history of skin cancer or family history of melanoma also correlated with likelihood that melanoma will be discovered first by dermatologist screening.
The study, published in the June, 2011 issue of the Archives of Dermatology, a Journal of the American Medical Association, concluded: “Screening and surveillance efforts should focus on patients 50 years or older and those with a personal history of skin cancer or a family history of melanoma.”
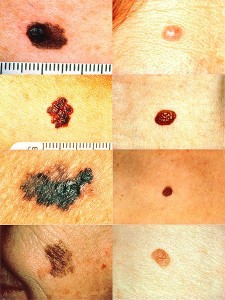
[Editor's Note: The image at left depicts melanomas (left side) vs. normal moles (right side).]
As an introduction to the study, lead study author, Laura K. Ferris, MD, PhD, of the Department of Dermatology, University of Pittsburgh School of Medicine, and her colleagues state:
“Melanoma outcome is strongly determined by tumor thickness at the time of diagnosis. As such, there is considerable interest in improving melanoma outcomes through regular examination of patients by dermatologists, which is assumed to detect early, thinner melanomas. However, specific screening and surveillance recommendations vary widely.”
The authors point out that other studies have found about half of all melanomas are first detected by the patient. However, they say that more information on “which patients are least likely to self-detect melanoma or to detect it only at a later stage, would be useful in making more pragmatic decisions regarding the benefits of skin cancer screening and surveillance recommendations.”
Therefore, in this new study, the researchers sought to determine which group of patients is least likely to self-detect melanoma, or to detect melanoma only at a later stage. They studied the records of 167 patients at the University of Pittsburgh Medical Center with cases of melanoma confirmed by biopsies between January 2003 and December 2008. They sought to measure the extent of any correlation between first detection by a dermatologist and factors such as the patient’s age, sex, tumor thickness when diagnosed, personal history of skin cancer, and family history of melanoma.
They found that 60.5 percent of the melanomas in the study were first discovered by the patients themselves. However, on closer examination, it was the younger patients who were most likely to self-detect the melanoma. Only 3 percent of all the melanomas in the study were first detected by dermatologists in those patients who were under 50 years old and low risk for skin cancer based on personal and family medical history.
However, the study found that dermatologists were most likely first to detect the melanomas found in patients 50 years old or older, and those who had a personal history of melanoma or any skin cancer. Approximately 50 percent of the melanomas in patients 50 years or older were detected by dermatologists, not by the patients themselves.
The researchers found it did not make a significant difference whether the patient over 50 was male or female, as to whether dermatologist-screening was most likely to first catch the melanoma. The significant factor was found to be the patient’s age, not gender.
The study also found that “Overall, dermatologist-detected melanomas were thinner than patient-detected melanomas, although in this study the difference was not statistically significant.”
Of all the factors studied, the researchers found, “being 50 years or older (OR, 2.69 [95% CI, 1.18-6.16]), personal history of skin cancer (5.69 [2.53-12.80]), and family history of melanoma (3.70 [1.29-10.60]) were all independently associated with dermatologist detection.”
The study authors note that there has not been agreement among medical authorities on the value of melanoma screening. For example, the US Preventive Services Task Force (2009) stated that there was not sufficient evidence to recommend for or against skin cancer screening. However, the American Cancer Society does recommend skin cancer screening as part of periodic health assessments in adults.
The researchers observe that cancer-screening, in general, has been shown to “have the highest yield of cancers detected per individuals [sic] screened when the screening is targeted toward higher-risk patients.” And, they state that “Consideration of which patients are least likely to detect their own melanoma is important when formulating melanoma screening guidelines.”
The authors caution that “clinical judgment should play a role in determining which patients should be screened regularly for melanoma.” Pointing out some limitations of their study, they note that because of their primary focus on the role of dermatologists, they counted as self-diagnosed both patients who found their own melanoma and those who presented at the dermatologist’s office after their melanoma was found by a spouse, friend, or primary care physician.
In conclusion, they write:
“In light of the average wait times of 38 days for an appointment to evaluate a changing mole, improved access to prompt evaluation of suspicious lesions is also an important part of melanoma secondary prevention.”
More Information
For more information on Skin Cancers, see our resource pages on Skin Cancers, which include sections on:
_____________
Copyright © 2011 Care-Help LLC












Recent Comments from our Online Community